Lupine Publishers | LOJ Medical Sciences
Abstract
Purpose: Here, we
report the complications of endoprosthesis with threaded cups according to our
application in cases of complicated acetabulum (hip revisions and
femoroacetabular impingement (FAI)).
Methods: A total
of 504 patients was analyzed, including 189 men and 315 women. For re-implanted
patients (n=49), the mean time to re-implantation was 6.3 years and the average
age at re-implantation was 54.7 years. For censored patients (n=455), the mean
time to censoring was 5.5 years and the average age of the implant was 55.7
years. Among the patients that were censored, 77 died and 378 patients did not
experience an event necessitating re-implantation.
Results: For the total
study population, the Kaplan-Meier estimate of 5-year survival is 0.94 and of
10-year survival is 0.85. 90% of the implants survived 7 years, 80% of the
implants survived almost 12 years and 70% of implants survived almost 15 years.
Kaplan-Meier survival analysis suggests that men have higher survival than
women. Age of the patient at the time of implant was not a statistically
significant factor for re-implantation (p value=0.21) but sex was (p
value=0.02). Women had 2.25 times more risk of being re-implanted than men.
Conclusion: In our
case series, the failure rate, as a result of aseptic loosening, was 7.4%
(n=51). More than half the failure cases (56%) required re-implantation. Over
one-third (37%) of the primary arthrosis cases, were found to be FAI, lessening
the frequency of diagnosis of the former. In our clinic, the threaded cup seems
to be indispensable in hip revision surgery and in treating FAI.
Keywords: Hip; FAI;
Conclusion
Acknowledgements
This article does not contain any studies with human participants or animals
performed by any of the authors.
Abstract
In our hospital, the most common indication for hip revision
surgery is post dysplastic arthrosis, followed by femoroacetabular impingement
(FAI), early progressive and deformative arthrosis of the hip joint and
protrusio acetabuli, with cases of achondroplasia or deformative arthrosis in
hereditary multiple exostoses being rarer but not uncommon. The cases of post
dysplastic arthrosis represent developmental dysplasia of the hip (DDH),
epiphyseal dysplasia, spondylo-epiphyseal dysplasia, and proximal femoral focal
deficiency (PFFD) or neurogenic luxation of the hip. In our experience, a small
portion of the patients requiring hip revision surgery have shown necrosis of
the femoral head, manifesting from chondrolysis of the hip joint, from coxitis
(including tuberculosis coxitis), from radiation therapy and from hemophilia.
In addition, we noted over time, that a small portion of rheumatic patients
were treated with the use of threaded cups.
In our experience, we have also noted that a portion of the
patients who were treated with threaded cups experienced complications. The
complication of posttraumatic arthrosis has not been uncommon, the conditions
of which involve slipped capital femoral epiphyisis, acetabular fractures
either treated conservatively or operatively, pseudoarthrosis after femoral
neck fractures or fusion of the hip joint. Cancer patients have represented a
distinctive group for postsurgical complications (including need for
re-implantations). The types of cancers related to the original hip revision
surgeries have been benign acetabular cysts, Hodgkin’s lymphoma, Ewing’s
sarcoma, and giant cell tumor or desmoplastic fibroma in the supra-acetabular
region. In our hospital, the ratio of primo-implantation to total implantations
has been relatively low and that of re-implantations has been nearly one-third,
making threaded cups irreplaceable in hip revision surgery at our institution.
In order to share the knowledge from our collective experience
with hip revision surgery using threaded cups for diverse cases, we performed a
systematic evaluation of the overall complications our patients have
experienced from hip revision over a 10-year period (2002-2012).
Materials and Methods
In the 10-year period of 2002-2012, a total of 565 patients underwent
hip revision surgery with threaded cups. Of those, 504 patients had complete
data and were selected for analysis (189 men and 315 women). The total study
population included 49 patients with re-implantation and 455 patients that were
censored. For the re-implanted patients, the mean time to re-implantation was
6.3 years and the mean age at the time of implant was 54.7 years. For the
censored patients, the mean time to censoring was 5.5 years and the mean age at
implant was 55.7 years (Table 1). Among the censored patients, 77 died and 378
did not experience an event necessitating re-implantation.
Table 1: Descriptive
statistics of time to event and age of the patient at the time of implant for
the study population. Data are presented in years.
Among the total study population, 16.8% had indication for primary arthrosis. In general, those patients were relatively younger and with early progressive and deformative arthrosis of the hip joint, hip arthrosis with protrusion, and FAI. We also recorded the numbers of achondroplasia patients or deformative arthrosis in hereditary multiple exostoses. When we selected 100 patients from among the group of primary arthroses cases, 37% were found to be FAI, indicating that FAI is secondary arthrosis in origin.
Figure 1: Representative
case of high iliac luxation – Hartofilakidis Type III, Crowe Type IV, Eftekhar
Type D hip dysplasia, solved with bilateral endoprosthesis (THR) and having visible
difficulties with stem implantations.
Figure 2: A patient
requiring hip revision surgery following septic coxitis with necrosis of the
head of the femur. The patient underwent THR. (a) 3-months post-operative. (b)
6-months post-operative. (c) Aseptic loosening of the cup detected at 9 months
follow-up. (d) Re-implantation with larger cup.
Rheumatic patients in our study population had received longterm corticoid therapy; among these patients, osteoporosis and necrosis of the femoral head is common. The threaded cup was used in 3.2% of this study subgroup. The rheumatic patient group also included several cases of ankylosing spondylitis (also known as Bechterev’s disease) and juvenile rheumatoid arthritis. Regarding the difficult anatomical acetabulum of these cases, 7.7% of the patients implanted with threaded cups experienced posttraumatic arthrosis, the conditions of which involved slipped capital femoral epiphyisis, acetabular fractures either treated conservatively or after osteosynthesis, pseudoarthrosis after femoral neck fractures or conditions after posttraumatic arthrodesis of the hip joint.
Among the total study population, rare indication was oncological
status (1.6%). Such cases consisted of benign acetabular cysts, Hodgkin’s
lymphoma, Ewing’s sarcoma, giant cell tumor or desmoplastic fibroma in the
supraacetabular region. When we compare threaded THR primo-implantations to
total number of primo-implantations at our institution in the 10-year study
period, there was an average 13.1% of primo-implantations. The same comparison
for the re-implantation group showed that we used the threaded THR 27.2% on
average, making this treatment modality indispensable in hip revision surgery
at our institution.
Figure 3: Representative
case of cup breakage due to loss of bone in the supero-lateral part of the
acetabulum affected with metastatic process.
We noticed aseptic loosening of the cup in 48 cases, of which 18 cups loosened after primo-implantation and 29 loosened after re-implantation, giving a failure rate of over one-half (56%). This high percentage is largely due to the area of implantation being technically difficult, which necessitated the use of a different device (i.e. the threaded cup); the rest represented failure of the cups after acetabular fractures (2 cases) and after metastatic affections surrounding the acetabulum (2 cases). Dislocations of the THR occurred in 4.4% (30 cases) of the study population, and 15 of the cups required operative intervention. In 5 cases, open reduction was enough; in 9 cases we re-implanted the inlay or head with one of a bigger size, and in 6 cases we performed re-implantation of the stem or cup to correct the position of the implant.
There were infectious complications in 3% (21 cases) of the study
population. In 17 of those cases, a revision procedure was required, including
5 revisions to address an early superficial infection and 2 revisions for deep
infection. Proper drainage with retained implant was achieved in all cases. A
total of 13 patients remain in follow-up to date, including 3 patients with
chronical fistulation, 8 patients who underwent two-stage re-implantation of
the THR, and 2 patients who underwent implant removal and had no further
re-implantation.
There was slow migration of the implant into the pelvis or up into
the iliac bone without obvious loosening in 2.3%. This migration is likely
explained by loosening of the circumferential grip of the cortical bone, when
the anterior and/or posterior acetabular wall is weakened. In such a condition
of cortical weakening, the underlying cancellous bone does not have enough
mechanical strength and thus the cup migrates (Figure 4).
Figure 4: Representative
case of slow migration up into iliac bone, with loosening at 8 years after the
primary implantation.
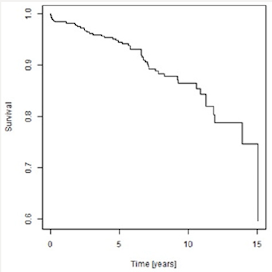
Graph 1: Kaplan-Meier
survivor analyses.
Considering the threaded cup concept, we have observed stress
shield effect often. Since the stress shield exerts its effect in cup
migration, focused follow-up is necessary to obtain meaningful findings. The
advantage of a threaded cup is that there is no need of full coverage. In
particular, 70% of coverage is sufficient, without need of augmentation [1]. In
addition, arthritis with protrusion (FAI pincer type) is one of the indications
for the threaded cup since those cases do not need support of the acetabular
floor. Implantrelated complications are to be considered as neuro-vascular
complications. Among our study population, there was a total number of 10 nerve
palsies (1.5%), 4 of which had to be operated; two of those patients underwent
sural graft transplantation due to femoral nerve cutoff, [2] and the other two
underwent the same procedure for static nerve palsy, with one requiring
simultaneous anterior tibial tendon transfer. In one case, we released the
lateral cutaneous nerve (Graph 1). The Kaplan-Meier survical curve suggests
that men have higher survival than women do (Graph 2).
Graph 2: Kaplan-Meier
survivor curve for men and women, showing the association of time to event to
sex.
Age of the patient at the time of implantation was not
statistically significant (p value = 0.21). Sex was a statistically significant
factor (p value 0.02). Women had 2.25 times more risk of being re-implanted
than men (Table 2).
Table 2: Cox model of
proportional hazard for patient sex, showing dependence of time to event with
age at the implant and sex.
Conclusion
Aseptic loosening reportedly occurs in around 6.5% of implanted patients at 4 years following placement [3]. In one study the radiological sign of instability was found in 21% of patients (n =130) at a mean follow-up of 3.9 years [4]. In another study [5], 17 cups (accounting for 25% of the cases assessed) were revised at an average of 5.2 years, with another 9 additional cases awaiting revision. Brujin et al. [2] reported migration for 25% of threaded cups in a follow-up of 4.5 years, and a 6% revision rate. It has been suggested that high and continuous stress near the threads may not allow bony in-growth [6] and may produce ischemia and necrosis [7] that require surgical revision in 14 months following the implantation surgery [8].
Discussion
Overall, 7.4% of our patients experienced loosening of the threaded cups and 3% experienced infectious loosening, which agrees with the literature [9,10]. In general, loosening of threaded cups does not give a good clinical and/or radiological outcome over the long term. X-ray appearance deteriorates with time, without evidence of an initial clinical correlation. The appearance of relative lines does not necessarily equate to the occurrence of loosening, but such a finding should be monitored carefully thereafter. Detection of osteolysis, however, indicates that loosening will occur [11]. A study by Harris et al from 1986 indicated that 79% of coxartosis cases originated from the cam impingement, with the rest by rheumatoid arthritis (21%) and hemochromatosis (10%).
In our series, when we compared 100 patients admitted for the THR
procedure, 37% showed FAI signs, with the average age of implantation being 58
years old. There were 23% post-DDH cases, 11% idiopathic avascular necrosis,
17% post-trauma cases, and 12% others; thus, the diagnosis of primary arthrosis
is much less common. FAI both types are finally resolved by a THR and indicated
much earlier than primary arthrosis. As changing in orientation of the
acetabuli we use these threaded cups, [12] more in pincer type of the FAI,
where orientation is essential. We don’t necessarily use these cups, though in
special cases we have to prefer primary stability to have good long-term
results. The failure of the threaded acetabular component is due to difficulties
of anatomy of the acetabulum, as observed in the cases in which we used this
component.
Even though we decided to use this special design of threaded cup,
despite its higher rate of complications, we were able to resolve one-third of
our re-implantation cases and to overcome the difficulties of the acetabulum in
FAI [13,14]. Kaplan-Meier survival curve analyses identified threaded cups as a
good option (with survival of 10 years); the Cox proportional curve indicated
higher risk for re-implant for women. Even though we investigated THR as a last
option for patients with FAI, pelvic transfers or any cervicocapital remodeling
may also represent last options. Ultimately, this study did not show the
threaded cup to be ideal for complicated acetabulum, though in our clinic it is
ideal for this diagnosis.
Read More Lupine Publishers Medical Sciences Journal Articles: https://lupine-publishers-medical-sciences.blogspot.com/







No comments:
Post a Comment