Lupine Publishers| Journal of Medical Sciences
Abstract
Melanoma is a type of skin cancer. Melanoma skin cancer is made up of
abnormal pigment cells (melanocytes). Melanocytes
are located at the bottom of the epidermis. These cells make melanin,
which spreads to the top of the epidermis and gives skin its
colour. Melanoma is usually brown or black in colour because the cell
still makes melanin. Melanoma is more dangerous than other
skin cancers because it more likely to spread if it is not found early.
However, most melanomas about 84 out of 100 are found early
before they have spread and so are likely to be cured with treatments.
Melanoma can occur on any skin surface. In men, it’s often
found on the skin on the head, on the neck, or between the shoulders and
the hips. In women, it’s often found on the skin on the
lower legs or between the shoulders and the hips. Melanoma is rare in
people with dark skin. When it does develop in people with
dark skin, it’s usually found under the fingernails, under the toenails,
on the palms of the hands, or on the soles of the feet. Although
one of the less common types of skin cancer, melanoma is considered the
most serious type of skin cancer because it is more likely
to spread to other parts of the body, especially if not detected early.
The earlier melanoma is found, the more successful treatment is
likely to be. Despite the many investigations in this field and a
rapidly growing knowledge base, classification according to specific
mutational profiles is not yet validated. Further investigations are
required for validation and refinement, and to possibly identify
additional factors.
Keywords: Melanoma; Melanocytes; Epidermis; Melanin
Introduction
Cancer is a disease of the cells, which are the body’s basic
building blocks. The body constantly makes new cells to help us
grow, replace worn-out tissue and heal injuries. Normally, cells
multiply and die in an orderly way. Sometimes cells don’t grow,
divide and die in the usual way. This may cause blood or lymph fluid
in the body to become abnormal, or form a lump called a tumour. A
tumour can be benign or malignant.
Benign tumour
Cells are confined to one area and are not able to spread to
other parts of the body. This is not cancer.
Malignant tumour
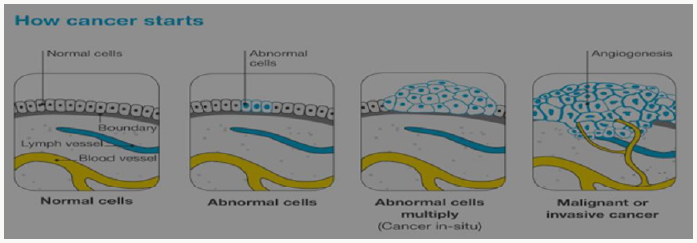
Figure 1: How cancer starts?
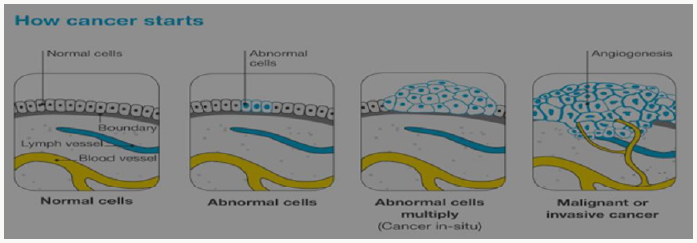
This is made up of cancerous cells, which sometimes also
have the ability to spread by travelling through the bloodstream
or lymphatic system (lymph fluid) (Figure 1). The cancer that
first develops in a tissue or organ is called the primary cancer. A
malignant tumour is usually named after the organ or type of cell
affected. A malignant tumour that has not spread to other parts of
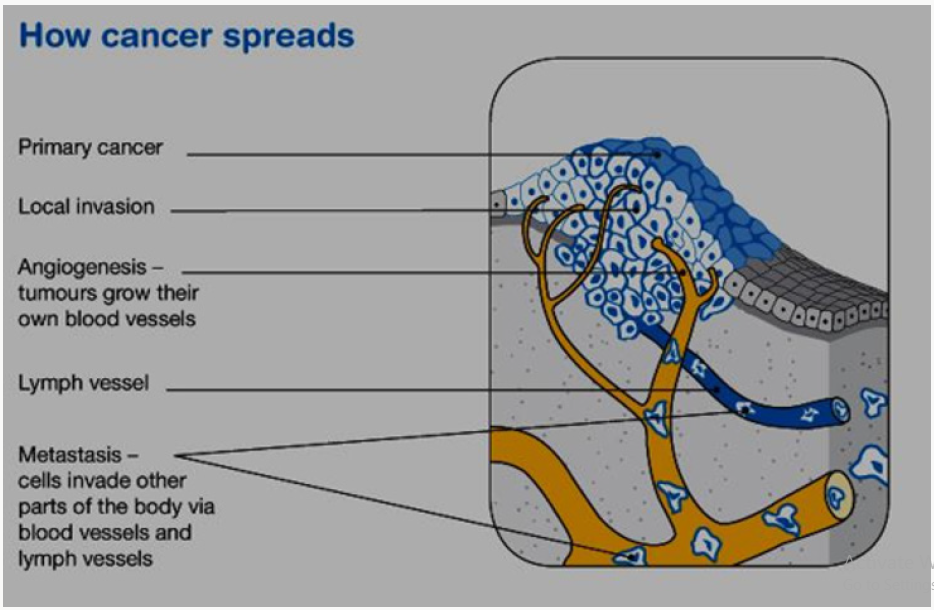
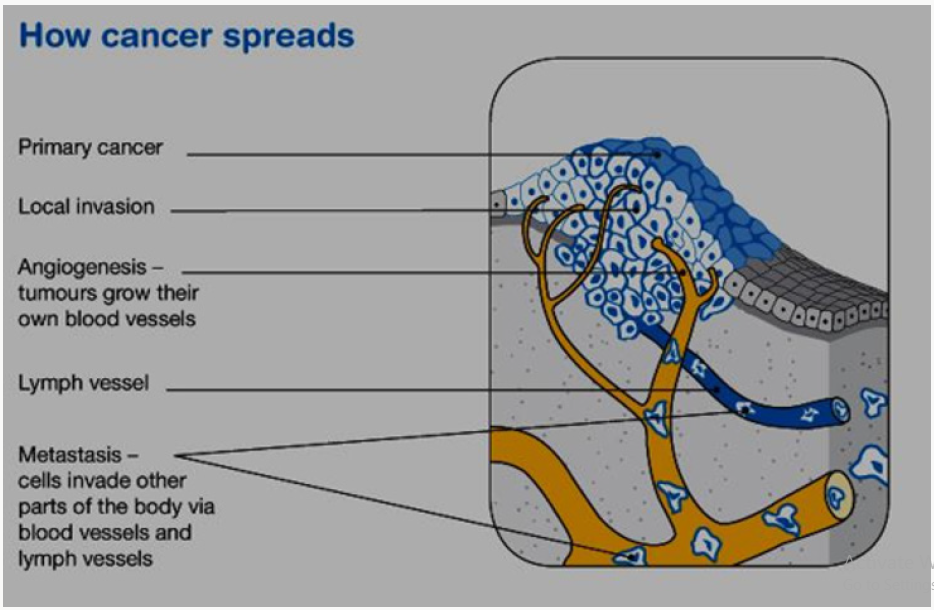
the body is called localized cancer. A tumour may invade deeper
into surrounding tissue and can grow its own blood vessels in
a process called angiogenesis. If cancerous cells grow and form
another tumour at a new site, it is called a secondary cancer or
metastasis. A metastasis keeps the name of the original cancer. For
example, melanoma that has spread to the bones is called metastatic
melanoma, even though the person may be experiencing symptoms
caused by problems in the bones (Figure 2).
Figure 2: How cancer spreads?
The skin
The skin is the largest organ in the body. It acts as a barrier
to protect the body from injury, control body temperature and
prevent loss of body fluids. Skin, like all other body tissues, is made
up of cells. The two main layers of the skin are the epidermis and
the dermis. Below these is a layer of fatty tissue (subcutis). The
epidermis is the top, outer layer of the skin. It contains three main
kinds of cells:
Squamous cells - These flat cells are packed tightly together
to make up the top layer of skin and form the thickest layer of the
epidermis. These cells eventually die and become the surface of
your skin. Over time our body sheds these dead skin cells.
Basal cells: These block-like cells make up the lower layer
of the epidermis and multiply constantly. As they age, they move
upwards in the epidermis and flatten out to form squamous cells.
Melanocytes: These cells sit between the basal cells of the
skin
and produce a dark pigment called melanin, the substance that gives
skin its colour. When skin is exposed to ultraviolet (UV) radiation
melanocytes make extra melanin to try to protect the skin from
getting burnt. This is what causes skin to tan. Melanocytes are also
in non-cancerous (benign) spots on the skin called moles or naevi.
Most moles are brown, tan or pink in colour and round in shape [1].
Melanoma
All cancers involve the malfunction of genes that control cell
growth and division. Most cancers are diagnosed in persons 55 and
older. The lifetime risk for cancer is approximately 50% for men and
approximately 33% for women.1 About 5% to 10% of all cancers are
clearly hereditary; the other 90-95% of cancers are not hereditary
but result from damage to genes (that is, somatic mutations)
due to internal factors (that is, hormones, digestion of nutrients)
or external factors (such as tobacco, chemicals, and sunlight).
Cancer treatment includes surgery, radiation, chemotherapy, and
vaccines. Some cancers are treated using various combinations
of surgery, radiation, and chemotherapy [2]. Basal cell carcinoma
and squamous cell carcinoma are the most common skin cancers.
The most serious common skin cancer is melanoma (malignant
melanoma), which arises from neural crest-derived melanocytes located in the epidermis or dermis of the skin. Melanomas also can
arise from melanocytes located in other regions of the body such
as the eye, meninges, digestive tract, or lymph nodes. Melanocytes
in the skin can give rise to a number of benign lesions such as nevi
(moles), dysplastic nevi, Spitz nevi, blue nevi, solar lentigo, and
seborrheic keratosis. When dealing with melanoma of the skin,
establishing which pigmented lesions are malignant is the prime
clinical problem, as the vast majority are benign.
Epidemiology and Aetiology
Exposure to the sun is the most commonly associated factor
[3,4]. Predisposing factors that have been found to increase the
risk of melanoma include skin that sunburns easily, poor tanning
response, light-colored skin, history of severe sunburns, numerous
nevi (more than 50), atypical nevi (that is, dysplastic nevi), a
tendency toward freckling, a history of skin cancer, a family history
of melanoma, the use of tanning salon, previous melanoma, and a
weakened immune system (due to other cancers, transplant drugs,
or HIV infection). Oral methoxsalen (psoralen) and ultraviolet A
radiation is an effective treatment for psoriasis, but it is carcinogenic
and increases the risk for melanoma. Individuals with recreational
and vacation sun exposure may be at greater risk than those whose
occupation exposes them to the sun constantly. In fact, continuous
sun exposure appears to be a protective factor where melanoma is
concerned.
Melanoma is a common cancer. In early 2005, the American
Cancer Society estimated that approximately 59,500 individuals
would be diagnosed with melanoma, the projected number
of deaths was 7,770. The prevalence of melanoma is 13:1,000
Caucasian Americans. During the 1970s, the incidence rate of
melanoma showed a marked increase of approximately 6.0%
per year, although this rate slowed to approximately 3.0% a year
beginning in 1981. There is some data to suggest that superficial
spreading melanoma has been found more frequently during the
last 30 years. Five-year survival rates for melanoma of the skin have
increased from 80% in 1976 to 85% in 1985 to 91% in 2000 [5].
Types of melanoma
Superficial spreading melanoma: It begins with an
intraepidermal horizontal or radial growth phase, appearing first
as a macule that slowly evolves into a plaque, often with multiple
colours and pale areas of regression. Secondary nodular areas may
also develop. This is the most common type of melanoma, making
up 55-60% of all cases. It is more common in younger people and is
often related to a pattern of irregular high sun exposure, including
episodes of sunburn. It can start as a new brown or black spot
that spreads within the outer layer of the skin (epidermis), or an
existing spot, freckle or mole that changes size, colour or shape. It
can develop on any part of the body. This type of melanoma often
grows slowly and becomes more dangerous when it invades the
lower layer of the skin (dermis) [6].
Nodular melanoma
Is a primarily nodular, exophytic brown-black, often eroded or
bleeding tumour, which is characterized by an aggressive vertical
phase, with a short or absent horizontal growth phase. This type
makes up about 10-15% of melanomas. It usually appears as a
round, raised lump on the surface of the skin that is often red, pink,
brown or black and feels firm to touch. It may develop a crusty
surface that bleeds easily. It is most commonly found in older
people on severely sun-damaged skin on the head and neck. It is a
fast growing and aggressive form of melanoma, spreading quickly
into the lower layer of the skin (dermis) [7].
Lentigo maligna melanoma: Arises often after many years
from a lentigo maligna (melanoma in situ) located predominantly on
the sun-damaged faces of older individuals. This type of melanoma
is most common in older people. It makes up about 10-15% of
melanomas and begins as a large freckle (lentigo maligna) in an area
of sun-damaged skin, such as the face, ears, neck and head. It may
grow slowly and superficially over many years before it penetrates
more deeply into the skin. Acral lentiginous melanoma: is typically
palmoplantar or subungual. In its initial intraepidermal phase
(which may be protracted), there is irregular, poorly circumscribed
pigmentation; later a nodular region reflects the invasive growth
pattern. This is an uncommon type of melanoma (around 1-2% of
all cases). It is most commonly found on the hairless skin on the
soles of the feet or palms of the hands, or under the fingernails or
toenails. It commonly appears as a colourless or lightly pigmented
area, which can be mistaken for a stain or bruise. In the nails, it
most often presents as a long streak of pigment in the nail or
discoloration in the skin around the nail. It may grow slowly before
it becomes invasive.
Desmoplastic melanoma
This is another uncommon type of melanoma (around 1-2% of
cases) that presents as a firm, progressively growing lump, often
on the head or neck. Many are skin-coloured and not pigmented
and can be difficult to diagnose. There are some other rarer types
of non-skin melanoma. Mucosal melanomas start in the tissues
in the mouth, nervous system, anus, urethra, vagina, and nasal
passages. Ocular melanomas start in the eye. Recent molecular
studies have shown the genetic heterogeneity of melanoma, with
distinct molecular signatures identified in tumours at different
anatomical locations and with different associations with reported
sun exposure.
Symptoms of Melanoma
Often the first sign of melanoma is a change in the shape, color,
size, or feel of an existing mole. Melanoma may also appear as a new
mole. Thinking of “ABCDE” can help you remember what to look for
a) Asymmetry: The shape of one half does not match the
other half.
b) Border that is irregular: The edges are often ragged,
notched, or blurred in outline. The pigment may spread into the
surrounding skin.
c) Color that is uneven: Shades of black, brown, and tan may
be present. Areas of white, gray, red, pink, or blue may also be
seen
d) Diameter: There is a change in size, usually an increase.
Melanomas can be tiny, but most are larger than the size of a
pea (larger than 6 millimeters or about 1/4 inch).
e) Evolving: The mole has changed over the past few weeks
or months.
f) Risk and prevention: Exactly what cause of melanoma
is unknown? But many risk factors for melanoma are known.
A risk factor for melanoma is known. A risk factor is anything
that increases the chance of getting a disease. Some risk factors
are passed down from parent to child through genes. Other
risk factors are activities that people do. Having one or more
risk factors does not mean you will get melanoma. Likewise,
melanoma occurs in some people who have no risk factors. Key
melanoma risk factors are described next.
g) Ultraviolet energy: Melanoma often occurs on parts
of the body exposed to UV energy. UV energy is an invisible
light energy. The main source of UV energy or rays is sunlight.
Tanning beds also expose the skin to UV rays and are known to
cause skin cancer, including melanoma. Both UVA (ultraviolet
A) and UVB (Ultraviolet B) rays contribute to the development
of Melanoma and skin cancer. Too much exposure damages
the skin and increases the risk for skin cancer. Whether sun
exposure was too much depends on UV intensity, length of
exposure, and how well the skin was protected [8].
Read More Lupine Publishers Medical science Journal Articles: https://lupine-publishers-medical-sciences.blogspot.com/